LEICESTER, United Kingdom – As England and Wales face the looming possibility of the legalization of assisted suicide, the Anscombe Bioethics Centre has launched its “Advance Decisions and Ethical Choices” Project.
It provides resources that are designed to guide users through the ethical and legal dimensions of advance planning of medical treatment, and to make decisions in accordance with Catholic moral teaching about end-of-life care.
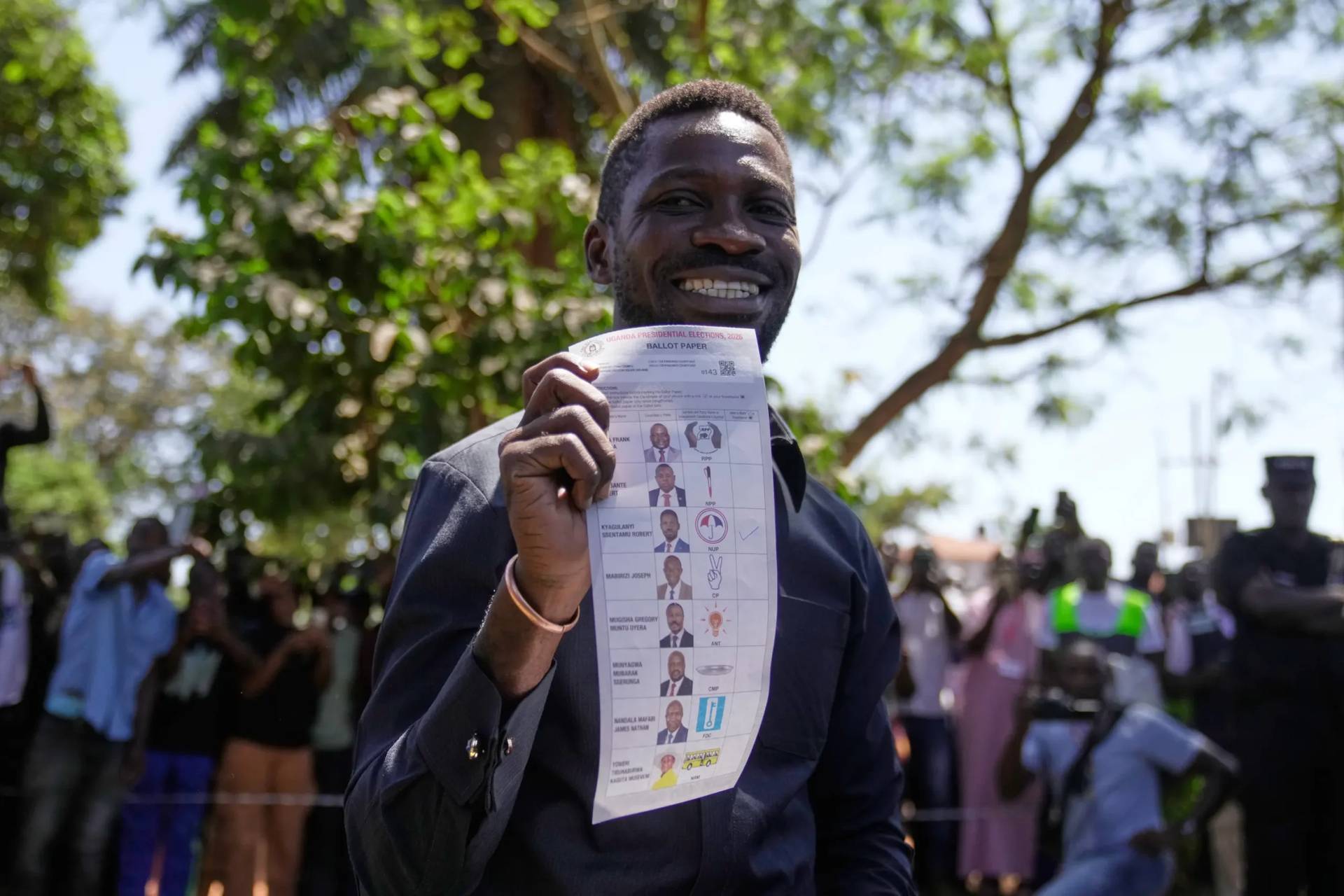
In June, the UK parliament House of Commons voted in favor of a bill to legalize assisted dying for terminally ill people, and will now be looked at by the House of Lords before becoming law.
“Many Catholics are often unsure about whether withdrawing life-sustaining treatment is equivalent to assisted suicide,” said Dr. Michael Wee, the Anscombe Bioethics Centre’s Associate Research Fellow.
“The Church teaches that it is not equivalent, provided the intention is not to end or shorten life, but to avoid overly burdensome treatment,” he told Crux.
“The same applies to advance refusals of treatment, with the caveat that it can be more difficult to predict when it would be appropriate to discontinue treatment in the future. Hence, our resources help users explore the different options available and think through what works best for their situation,” Wee said.
“If assisted suicide is legalized in the UK, it is important that we continue to draw a sharp distinction between assisted suicide and legitimate advance planning of treatment. Many people find it reassuring to make such plans, whether it’s a legally-binding advance refusal of treatment, a general statement of preferences, or giving someone they trust the power to make decisions for them,” he explained.
“It gives them comfort to know that their values will be respected and that they do not have to accept every single treatment at the end of life, whatever the risks or burdens. This is a good thing, and it should be facilitated, while also ensuring that such decisions respect the intrinsic dignity of life. That means avoiding blanket refusals of treatment, for example, and considering what level of flexibility their situation requires,” Wee told Crux.
In announcing, the new project, Wee said the toolkit put out by the Anscombe Bioethics Centre is designed to help people think about and make such decisions in a way that is both in accordance with the law in England and Wales “as well as in accordance with the moral values of the Catholic faith.”
He noted three tools are in place to deal with end-of-life care for those unable to make decisions: The advanced statement, a lasting power of attorney, and the advanced decision to refuse treatment.
“The first tool is the advanced statement, which is perhaps the most flexible document of the three,” Wee said.
“It is for stating your preferences, values, and beliefs about medical treatment. It could be a very specific statement or a very broad one. But importantly, the advanced statement is not legally binding. And this can be very helpful because it is often difficult to predict exactly what situation we will be in and what treatment options will be offered to us,” he explained.
“A lasting power of attorney – or LPA – is the second tool available. It means giving somebody else the power to make decisions on your behalf about treatment,” he continued.
“This power will only apply when you have lost mental capacity to make that specific decision. An LPA can be a good option if there is somebody in particular who is close to you and whom you can trust to be around and to advocate for your values and your preferences when you have lost mental capacity,” he said, adding this could be a friend or a family member.
He emphasized that an LPA only comes into effect when a person has lost mental capacity and can be broad or more specific.
“But the main thing is that the LPA offers both that flexibility and the assurance that there will be somebody you know who will be there to advocate on your behalf to your medical team,” Wee said.
He said the third tool is the advanced decision to refuse treatment, which is actually legally binding – unlike the two other tools.
“It has to be about a specific treatment that you refuse in advance in relation to specific circumstances that you detail in your document. Because it is legally binding, that means that should you lose capacity and those circumstances become a reality, then doctors are legally obliged to follow your refusal of that specific treatment named in your advanced decision,” he said.
“Because it is such a serious and powerful document, the advanced decision to refuse treatment should only be used when there is a serious and obvious need, such as when somebody has a progressive condition and it is relatively easy to predict the trajectory of that condition and what treatment options will be offered,” he continued.
“It’s important to say that you don’t have to use any of these tools as even if you don’t have any of them in place, doctors are still obliged by law to make decisions on your behalf in your best interests,” Wee added.
The Centre’s Director, Professor David Albert Jones, said the tool will play an important role in dealing with often troubling medical issues.
“The tools generated by this Project are thorough and comprehensive, and they are also accessible to a wide range of people who will need them. I am confident that they will be a lasting contribution to the Church and the wider community in this area of bioethics,” he said.
The Anscombe Bioethics Centre is closing down, but the tool will be available online for free after this happens.
Follow Charles Collins on X: @CharlesinRome